SITUATION:
This QuickHit was informed by Connected Care’s expansion of services to include ostomy education for family caregivers and home and community care providers.
BACKGROUND:
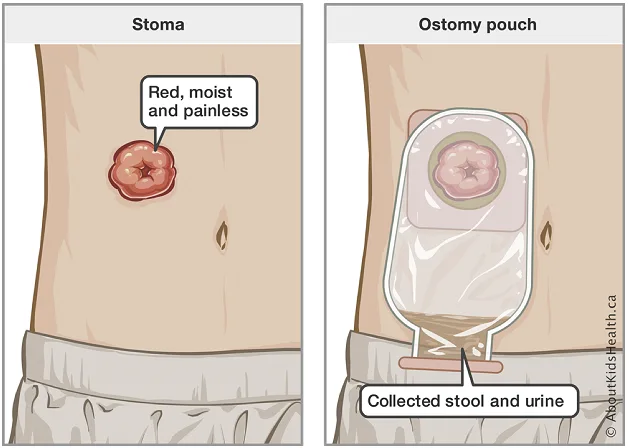
Children with medical complexity may have an ostomy to help with urine or stool elimination if their intestine or urinary tract does not work properly. An ostomy is an opening from the inside of the body to the outside, through the abdomen (tummy). It is created during surgery and it can be temporary or permanent depending on the child’s medical condition.
The end of an ostomy is called a stoma and is where urine or stool a exits the body. There are no nerve endings in a stoma which means the child cannot feel any sensation when it is touched or when urine or stool exits through it. The output (sometime called effluent) of a stoma is collected in a bag called an ostomy pouch. The pouch is waterproof, odour proof and protects the skin around a child’s stoma while keeping their clothes from getting dirty.
It is important to assess the stoma and its output to identify signs of potential complications that children with ostomies could experience.
ASSESSMENT:
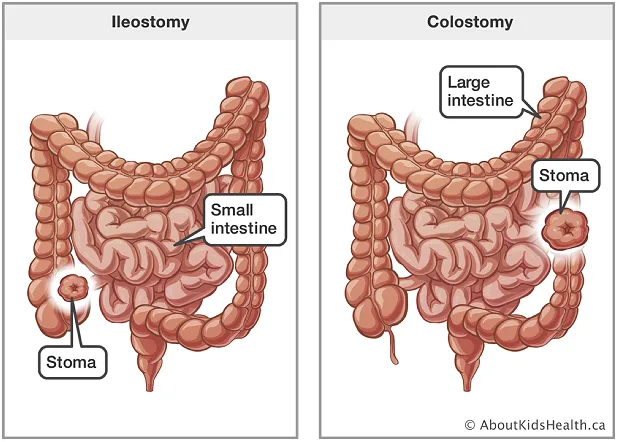
Ostomies have different names and depending on where they are located:
- Ileostomy: creates an opening that connects the last part of the small intestine (the ileum) to the abdomen
- Colostomy: creates an opening that connects the colon (large intestine) to the abdomen
- Urostomy: creates an opening that connects part of the urinary tract to the abdomen
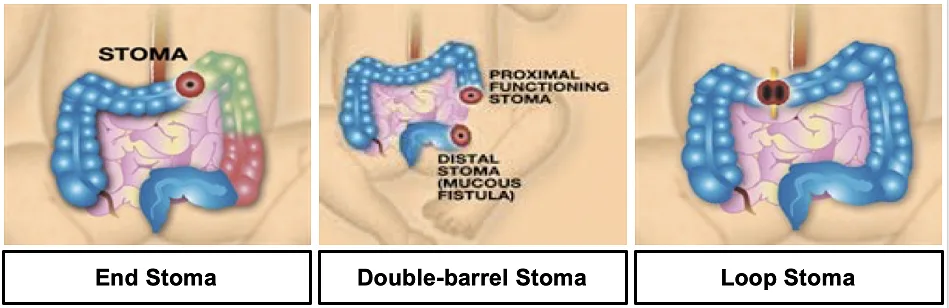
A stoma may also look different depending on how the ostomy was surgically created, as outlined below.
- End Ostomy: An end ostomy is created when the intestine is divided into two separate pieces, and the part of the intestine that is coming from the direction of the mouth is brought outside the abdomen. The other end is sewn closed and left inside the abdomen.
- Double-barrel Ostomy: A double-barrel ostomy is created when both ends of the intestine are brought outside of the abdomen. One stoma will drain stool, and the other will drain mucous.
- Loop ostomy: A loop ostomy is made by bringing a loop of intestine through the abdominal wall. A rod or ring is placed under the loop between the skin and the loop. This rod or ring will typically be removed by the child’s medical team within the first month.
RECOMMENDATION:
Connected Care recommends the following considerations when performing stoma assessments on children with ostomies in home and community settings:
- A stoma can look different in each child however, the general appearance is usually round or oval, red (like the inside of your mouth), moist and shiny.
- It can be normal for stomas to bleed when they are cleaned or touched. To stop bleeding, apply gentle pressure to the stoma with a cloth.
- Perform a comprehensive stoma assessment daily and as needed. The table outlined below can be used to guide a stoma assessment.
| Assessment | Normal Findings | Abnormal Findings |
|---|---|---|
| Colour | Beefy red or pink | Dark, black, blue, purple, pale |
| Appearance | Moist and shiny | Flaccid, dry |
| Shape & Size | Varies in the first 6-8 weeks after surgical creation. Can be round, oval or irregular. | |
| Height | Ideal is 1-2cm above skin level | Prolapse (stoma height above skin increased) or retraction (stoma is at or below skin level) |
| Effluent (output) | Ileostomy = Liquid porridge consistency Colostomy = Soft formed, toothpaste consistency Urostomy = Urine | ++ liquid output (ileostomy), foul smelling output, little to no output, blood in output |
| Peri-stomal skin | Free of redness or irritation. Skin can only be assessed when pouch is off. | Ulceration, excoriation, yeast pinpoint rash, separation between skin and stoma |
| Os (Where stool/urine exits the stoma) | Centre of stoma | Tilted to any other direction that can cause leakage |
- Contact/advise family to contact child’s health-care provider and/or Wound, Ostomy, & Continence (WOC) Nurse if you notice:
- Changes in appearance of the stoma, and it is affecting drainage
- The stoma is bleeding more than a small amount or will not stop bleeding
- Stoma retraction below skin level or protrusion above the skin
- Narrowing of the hole where stool or urine comes out from in the stoma that impacts drainage
- Changes to the amount or consistency of output
- Difficulties with pouch adherence on the skin (e.g., increase in leakage)
- Difficulties with skin, such as rashes, due to leakage from the ostomy pouch
- Partner with child’s family and seek medical attention at the nearest emergency department if:
- The stoma changes colour—e.g., the stoma becomes dark, black, blue, purple or pale
- The child is not peeing or has low output in their pouch
- There is a considerable increase or decrease in stoma output over a few hours
- There is blood in the pouch
- There is new redness, swelling, pain, pus or foul smell from the stoma or incision
- The child’s belly becomes painful, firm, and bloated
- The child has a fever of 38.3°C (102°F) or higher
- The child is crying non-stop or otherwise seems to be in pain
- The child has a green vomit, even once
- The child is unusually sleepy
More Information
Review the AboutKidsHealth Ostomy Learning Hub for more information about ostomy care.