SITUATION:
This Quick Hit comes from updated best practice guidelines regarding administering subcutaneous injections in the paediatric population.
BACKGROUND:
Subcutaneous injections are used to deliver a variety of medications common to paediatric populations in home and community care (e.g. low molecular weight heparin, insulin, GCSF).
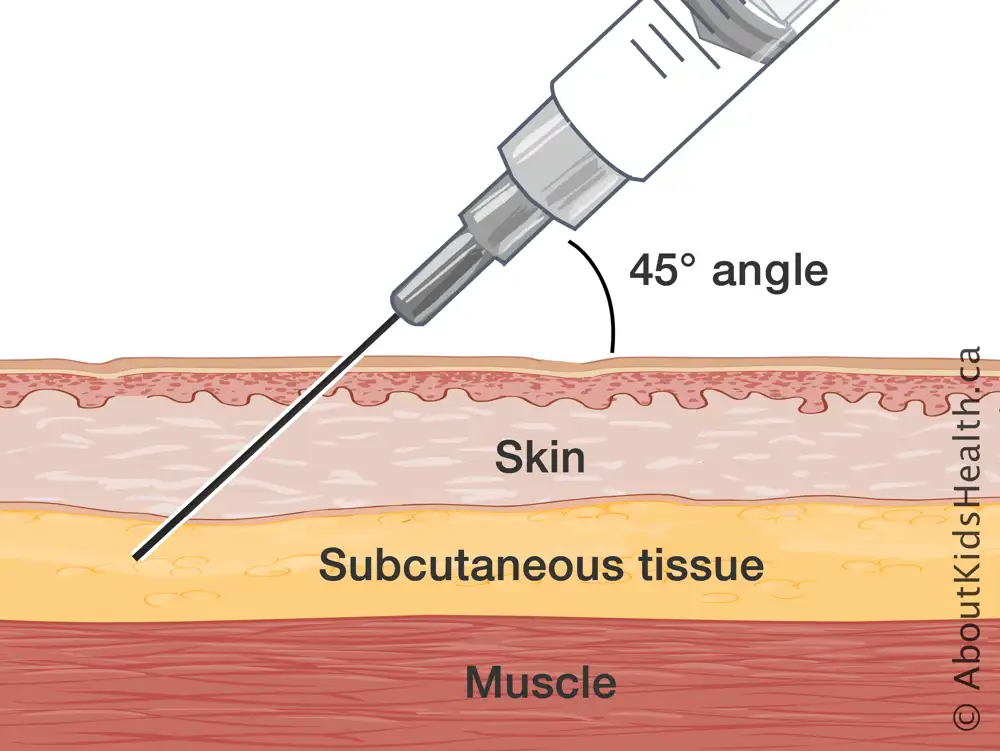
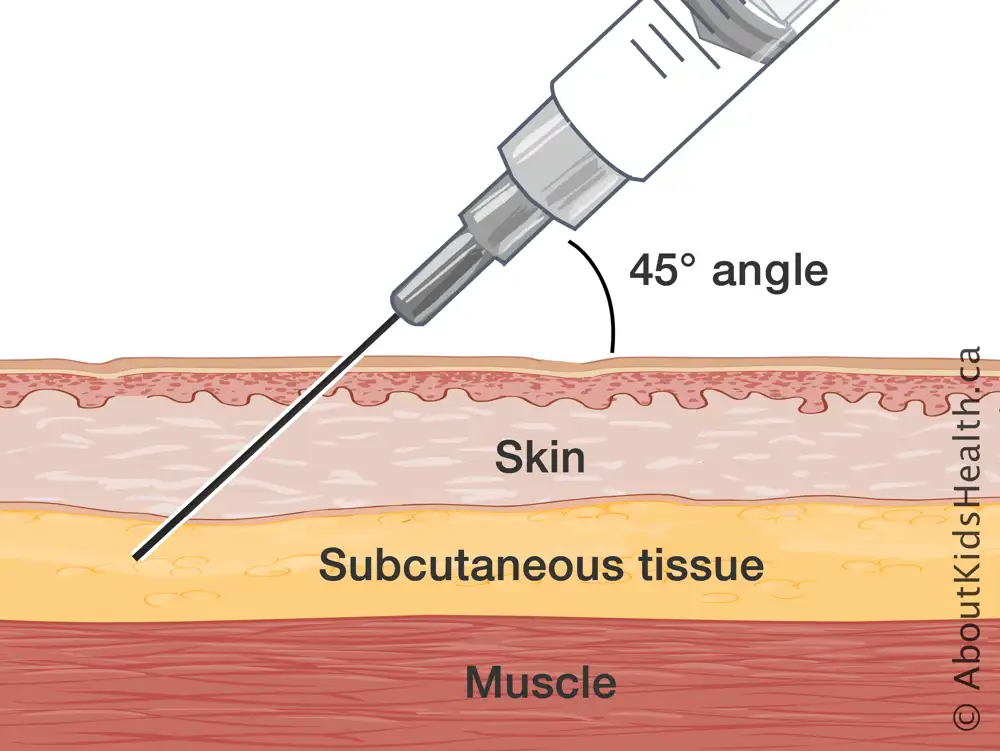
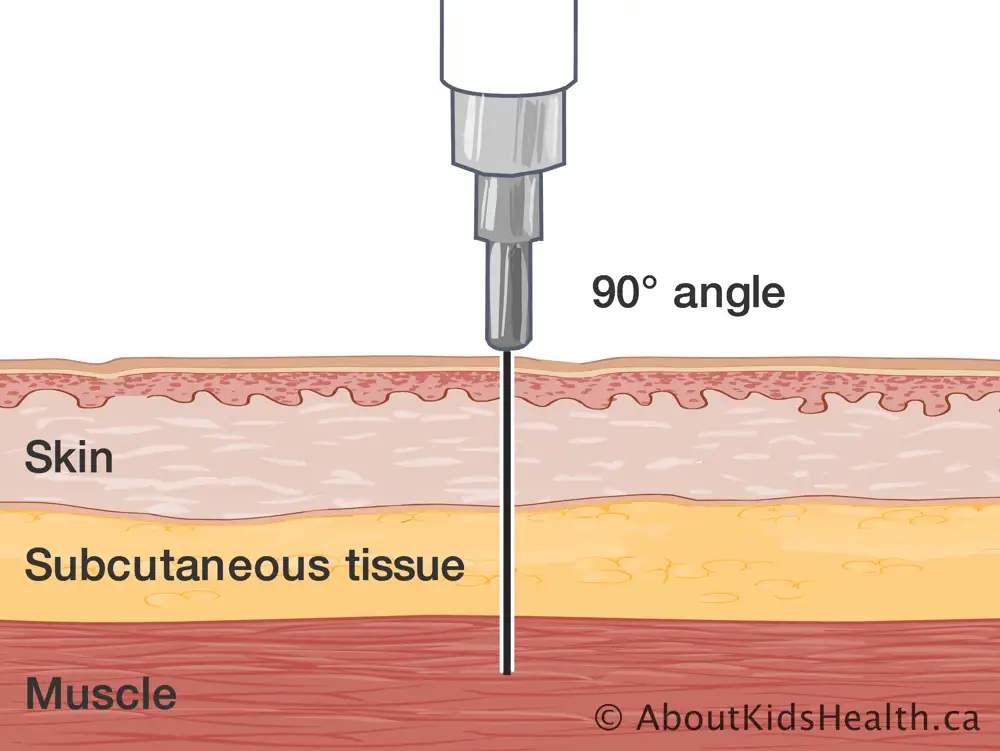
Subcutaneous injections are administered using a small needle, to deliver medication just beyond the epidermis and into a fatty layer of subcutaneous tissue where it is absorbed slowly over a period of time.
Best practice guidelines for injection techniques have been updated to address the challenge of delivering medications into the subcutaneous tissue for young children.
ASSESSMENT:
Selecting the correct supplies, site and method of administration of a subcutaneous injection will minimize complications and improve a child’s comfort with the procedure.
Prior to performing a subcutaneous injection, partner with the child or family caregiver to explore strategies to prevent needle poke pain and promote comfort, such as comfort positioning, skin numbing agents or distraction.
RECOMMENDATION:
Connected Care recommends following the most up-to-date best practice for administering subcutaneous injections. This includes the following care considerations:
- Use a needle no larger than 25 gauge in diameter and no longer than 16 mm in length.
- Select an appropriate injection site. Reference the following AboutKidsHealth article for more information.
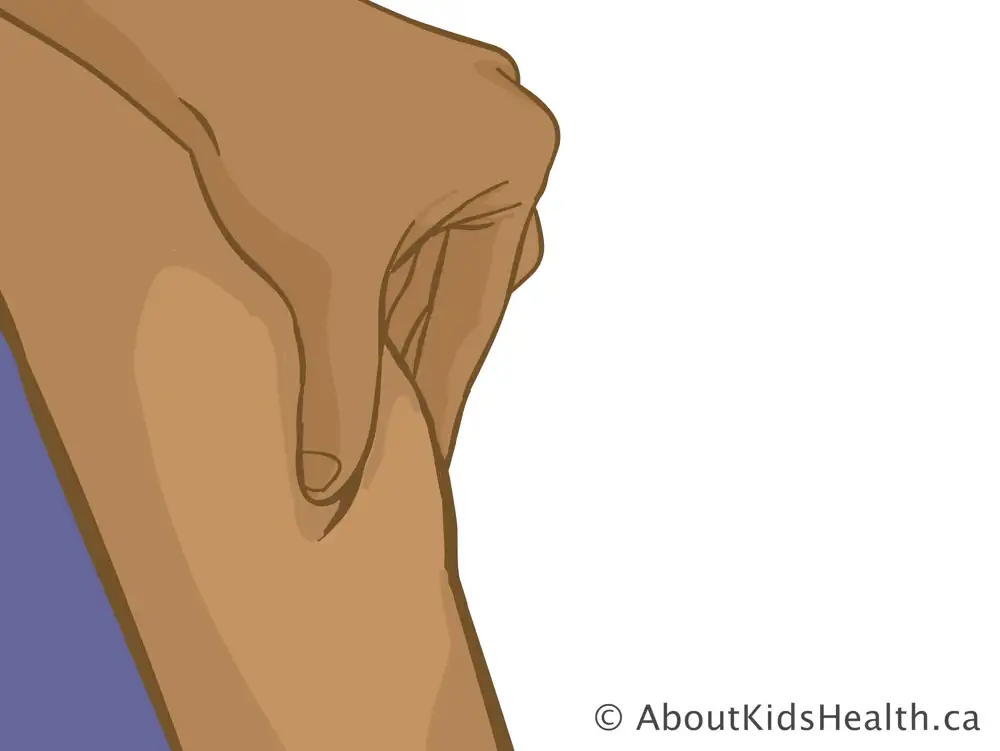
- Pinch up the fatty (subcutaneous) tissue while administering to prevent injection into the muscle.
- Use clinical skill and judgement when deciding on angle of insertion to prevent injection into the muscle in slimmer limbs and abdomen.
Reference these AboutKidsHealth articles for more information on Subcutaneous Injections and common subcutaneous medications